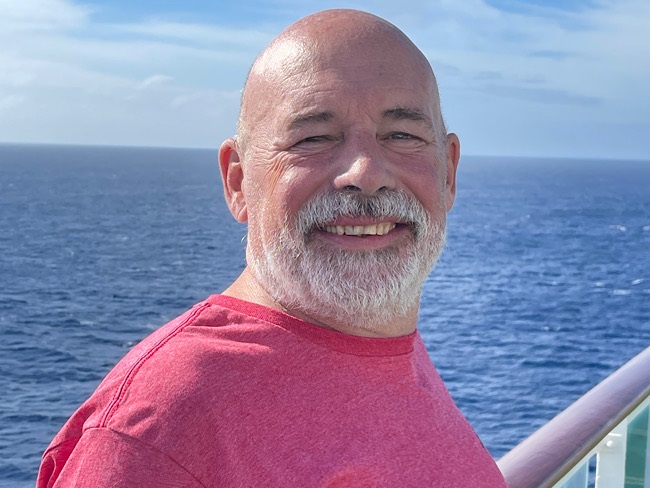
For a father with prostate cancer, knowledge is power
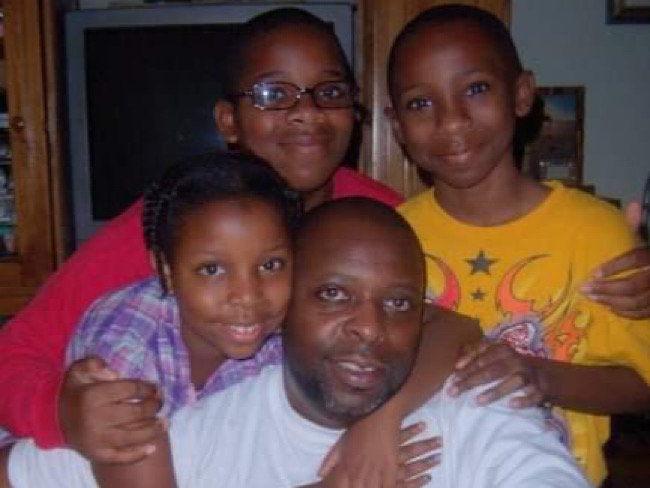
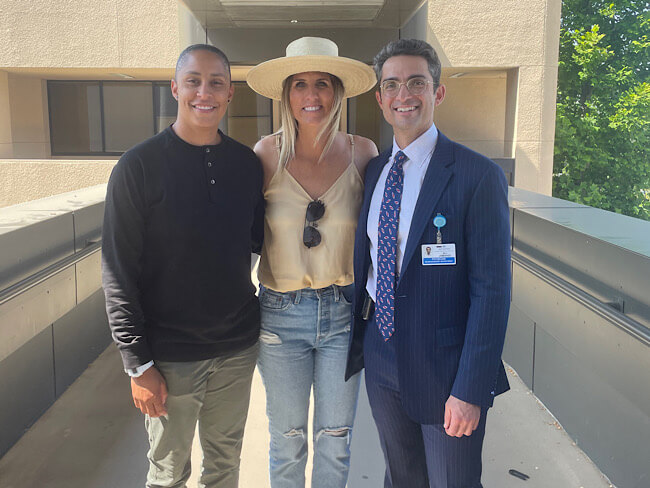
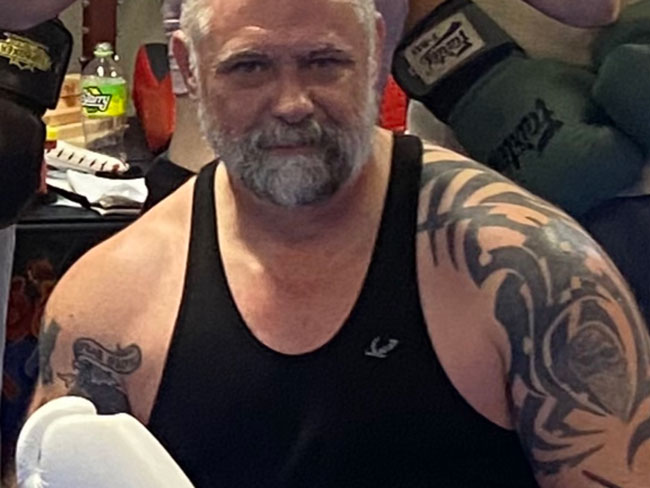
Harold Newman had advanced prostate cancer. Genetic testing helped expand his future treatment options and protect the health of his family members.
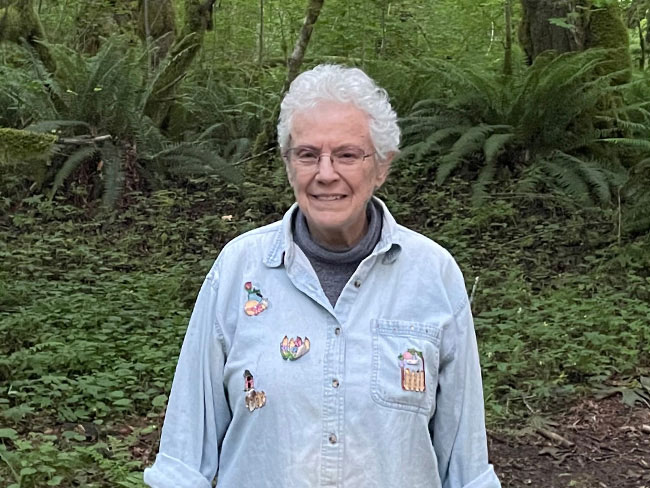
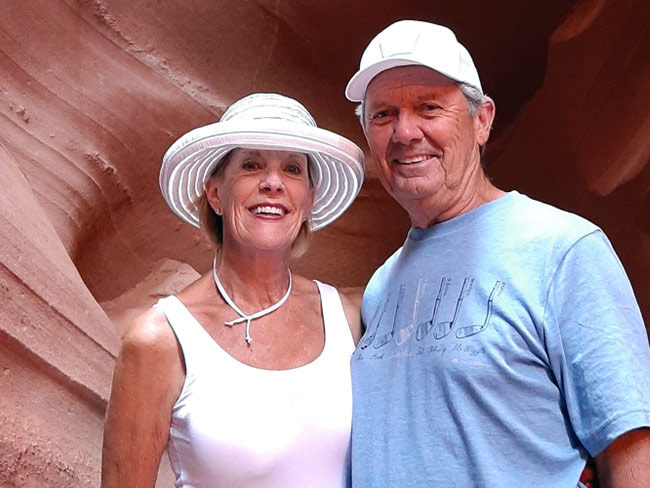
Newman’s successful treatment allowed him to continue pursuing his passions: hiking, birding, succulent gardening, and spending time with his family.
As a retired doctor, Harold Newman knew he needed to see a doctor when he noticed that he was urinating more often than usual.
He assumed the cause was an enlarged prostate gland. As men age, the prostate often gets bigger. This can cause a frequent or urgent need to urinate. A prostate-specific antigen test, or PSA test, is often used to determine if you have an enlargement, infection, or cancer of the prostate.
“Even though I didn’t have any other symptoms, my doctor ordered a PSA test to rule out prostate cancer,” said Newman, a Kaiser Permanente member who was 70 years old at the time. “This turned out to be a critical step, because my PSA levels were really high.”
Further testing revealed Newman had prostate cancer. The cancer had spread to the lymph nodes in his pelvis.
Symptoms can be mild or nonexistent
The most common symptom of prostate cancer is difficult or painful urination. When prostate cancer spreads, patients may experience bone pain, weight loss, or swelling in their legs and feet.
But it isn’t uncommon to have very mild symptoms, as in Newman’s case — or even to have no symptoms at all.
Prostate cancer can be difficult to detect and diagnose. Newman felt extremely lucky that his care team discovered the cancer when they did.
Consulting with a team of specialists
Because the cancer had spread beyond his prostate, Newman’s doctors didn’t recommend surgery.
10%
of prostate cancers are related to inherited gene mutations
Instead, he first received a hormone-blocking drug to stop his body from producing testosterone. Most prostate cancer cells feed on testosterone. Reducing testosterone levels can cause cancer cells to die or grow more slowly.
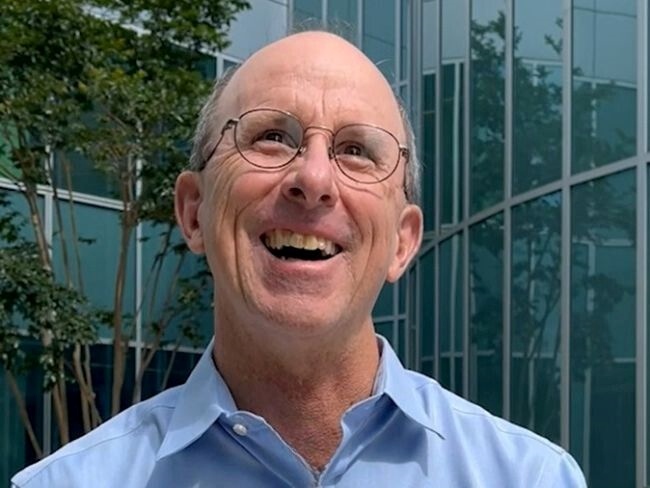
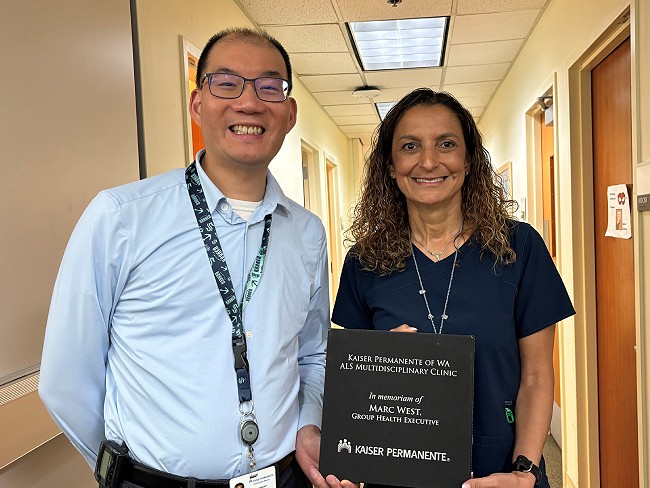
Andrea Harzstark, MD, a genitourinary medical oncologist at the Kaiser Permanente San Francisco Medical Center, also recommended targeted radiation therapy to destroy cancer cells.
This combination of treatments was successful. Newman’s cancer was no longer detectable, and his PSA levels returned to normal.
Genetic testing can help identify targeted treatment options
Newman’s care team also recommended genetic testing since about 10% of prostate cancers are related to inherited gene changes, called mutations.
If a genetic test shows that a patient has a certain mutation and we only learn years later that it’s significant, our genetics team has a mechanism that enables them to go back through patient records and identify everyone who could benefit from this new knowledge.” Andrea Harzstark, MD
He learned he has a BRCA2 mutation. (Pronounced “BRAH-kuh,” BRCA is short for BReast CAncer.) BRCA mutations can be passed down through families.
“Mutations in the BRCA1 and BRCA2 genes are much more well-known for increasing the risk of breast and ovarian cancer,” Dr. Harzstark explained. “But we’ve learned that they play an important role in prostate cancer, as well.”
Genetic testing can help identify targeted treatments for people with cancer. Some patients benefit right away, and some benefit years after their original diagnosis and treatment.
“If a genetic test shows that a patient has a certain mutation,” Dr. Harzstark said, “and we only learn years later that it’s significant, our genetics team has a mechanism that enables them to go back through patient records and identify everyone who could benefit from this new knowledge.”
For example, in 2020, 4 years after Newman’s diagnosis, a category of drugs called PARP inhibitors was approved by the FDA as an effective medicine for patients with a BRCA mutation and advanced prostate cancer.
Even though his initial treatment was successful, Newman feels even better knowing that there’s another effective treatment available if his prostate cancer comes back.
Genetic testing can help protect your family’s health
Newman’s genetic testing also provided valuable information for his family, including 2 children in their 40s. After learning that their father had a BRCA2 mutation, both were advised by their Kaiser Permanente care teams to get screened.
His daughter’s test was negative. But his son learned that he too has the BRCA2 mutation. Because of his increased risk, he’s taking steps to safeguard his health. He’ll get regular screenings for the types of cancer related to BRCA2. If cancer develops, the aim is to detect it early, when it’s far easier to treat.
“This is why genetic testing is so important,” Newman said. “It expanded my treatment options, and it’s protecting my family’s health, too.”
If you have a family history of prostate cancer, ask your doctor whether genetic testing or earlier screening might be right for you.
Learn more about cancer care at Kaiser Permanente